Utah is home to 14 community health centers, operating 60 clinics in urban and rural communities to provide care to more than 166,000 people annually. Utah health centers foster trusting relationships with their patients and provide medical staff with the support they need to deliver the right care for patients. Medical doctors (most are family physicians) and advanced practice providers are the leads of healthcare teams where everyone works together to ensure the best patient care. Utah family physicians lead and practice across the state in these unique independent practices.
Health Centers: Caring Since 1965
In 1965, the nation’s first community health centers were launched as a small demonstration program by President Johnson’s Office of Economic Opportunity (OEO). Dr. H. Jack Geiger and Dr. Count D. Gibson had roots in both the civil rights movement and the War on Poverty and wanted to provide healthcare that could transform underserved communities.
The first “Neighborhood Health Centers” were established in Columbia Point in Dorchester, MA, an inner city, underserved community, and in Mound Bayou, MS, an impoverished rural community. These two centers provided care that was unconventional at the time by focusing on patients’ social drivers of health in addition to providing healthcare services. This demonstration program became today’s Health Center Program, which now serves over 30 million patients annually through 1,370 health center organizations.

What is a Community Health Center?
Health centers are community-based organizations that deliver high-quality primary health care services. Designed to be a true “Medical Home,” health centers provide access to pharmacy, mental health, substance use disorder (SUD) and oral health services in addition to primary care. You will find these clinics in areas where economic, geographic or cultural barriers have limited access to affordable healthcare services. Health centers care for the nation’s most vulnerable individuals and families, including people experiencing homelessness, agricultural workers, residents of public housing and the nation’s veterans. As a family doctor, you work with a team staffed and dedicated to the whole person.
How Do They Work?
Health centers overcome barriers to care by focusing on their community. Each health center has a Board of Directors with patient majorities, ensuring that community voices are heard and health centers remain responsive to local needs. Family physicians working in health centers are guaranteed variety in their scope of practice as each community has different needs. Some are full-spectrum with hospital and office-based practices; others are mobile, working in street medicine practices. Health centers can be large or small. In Utah, they are all private or public non-profits.
Health centers receive federal grant funding from the Health Resources and Services Administration (HRSA) to support the care they provide for low-income uninsured patients, but most of their operating funds come from patient revenues, including Medicaid, Medicare, private insurance and patient fees. Uninsured patients are charged on a sliding fee scale based on family size and income. Health centers measure the quality of care for patients and report regularly to their Boards of Directors and funders.
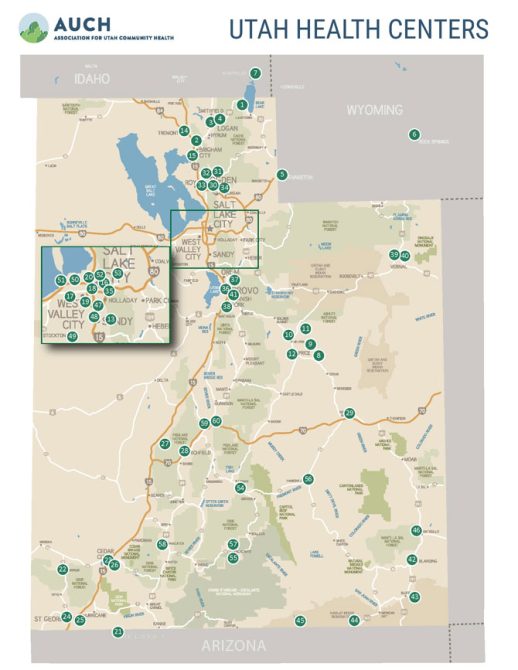
Utah’s Community Health Centers
Utah Health Centers are perfect places for family physicians to thrive as they support families and communities. Not only focused on what happens in the four walls of a clinic, Utah health centers address social drivers through care coordination, health education, assistance accessing insurance coverage and healthy lifestyle coaching. Many clinics have community health workers as part of their teams. Preventing illnesses and managing chronic disease creates value by providing care in the least costly setting and keeping people out of emergency rooms and hospitals. Utah health centers, by design, deliver integrated care where primary care and behavioral health clinicians work together with patients and families.
Most Utah health centers participate in centralized data reporting through a common population health platform, allowing them to benchmark with other centers to improve care, participate in value contracts, and manage high-risk cohorts. The platform has also allowed advances in enabling health information technology research projects with partners like Huntsman Cancer Institute Center for Hope to automate referrals for tobacco users to Utah’s Tobacco Quit Line and recall patients for preventive screening exams.
Utah Health Center providers are almost always eligible for loan repayment programs through the National Health Service Corps, Utah’s Healthcare Workforce Loan Repayment Program or both. The Association for Utah Community Health (AUCH) and the Utah Department of Health and Human Services have information about these programs for people interested in a career at a Health Center.
Click the link below to learn more about Utah’s community health centers.
https://www.auch.org/community-health-centers

Health Center Program Fundamentals:
- Deliver high quality, culturally competent, comprehensive primary care, dental, behavioral health, substance use disorder treatment, and access to affordable medications.
- Provide supportive services that promote access to health care such as health education, translation, and transportation.
- Provide services regardless of the patient’s ability to pay and charge uninsured patients for services on a sliding fee scale.
- Operate as autonomous community-based organizations directed by patient-majority governing boards.
- Develop systems of patient-centered and integrated care to meet the unique needs of their communities.
- Meet stringent administrative, clinical, and financial requirements.
Light at the End of the Tunnel: Newly Minted Family Medicine Doctors Start Their Practice
Cameron Smith, DO, and Matias Calquin, MD, are graduates of the Utah Valley Hospital Family Medicine Residency and have both started their family medicine jobs at Mountainlands Community Health Center in Provo as of July 2023.
Smith is from Utah and was looking to return to Utah for residency after time at Campbell University in North Carolina. He chose family medicine because it was the specialty that allowed him to follow his patients over time and develop relationships. In residency, he recalled the experience of providing prenatal care and attending two births for a family he cared for longitudinally. This was the most satisfying aspect of training, and he wanted to ensure that was a part of his career. He was also looking for a job where he might practice to the full scope of his training, including obstetrics. Smith met the family physicians from Mountainlands when he did his labor and delivery rotations in residency. He then worked in the Mountainlands clinic space as a volunteer in their free clinic. He ultimately rotated at Mountainlands to see if it was a good fit. “It was a no-brainer. Mountainlands has a close-knit family atmosphere and my colleagues here are close,” said Smith.
Calquin says he “came late” to an interest in family medicine. As a third-year medical student at the University of Utah School of Medicine, he did his third-year rotation at Mountainlands Community Health Center. He worked closely with Dr. Bruce Grover, Family Physician and Medical Director. He “fell in love” with being in the clinic and doing obstetric and nursery care at the hospital. He realized this was “why I went into medicine” and matched at Utah Valley Hospital’s fantastic residency. He practices obstetrics and sees babies in the nursery, taking calls with Smith and Dr. Grover, and they are expanding access to vasectomies at Mountainlands in addition to their outpatient practices.
Calquin’s first language is Spanish, and he is committed to serving patients that speak Spanish. His family had care at Midtown Community Health Center in Davis County, so he knows the importance of meeting the needs of this community with excellence.
Both Smith and Calquin are National Health Service Corps (NHSC) loan repayment recipients, and both appreciate that award. They plan to be at Mountainlands for a long time and anticipate developing increased teaching opportunities for students and residents.


“Quiet Leader”
Addie Slack, MD, is the Medical Director at Community Health Centers, Incorporated (CHC, Inc.). Her path to family medicine started early. She was exposed to rural family medicine in her small town of Edwards, CO. Her own family doctor was a model and a mentor; not only did he care for her and her family, but allowed her to participate on international care trips to Honduras as she was a budding premed.

Slack was a Spanish-language major in college and then attended Medical School at the University of Illinois at Rockford and residency at the University of Colorado in Denver. The Spanish language was formative in Slack’s ultimate path to working for CHC, Inc. She fell in love with the language and the added connection she was able to experience when she cared for populations that were primarily Spanish-speaking. She was also a National Health Service Corps Scholar, and job decisions had to include her eligibility to serve in a qualified setting. CHC, Inc. was lucky to get her in 2015.
Why did she choose family medicine? Slack shared, “I wanted a job where I worked with people and used my brain and science. And I realized I get bored with routine. Family medicine is always allowing me to learn and do something different. That is why I continue to practice obstetrics and nursery care. Continuity with my patients and relations are also key.”
Slack began to take on leadership positions in 2017 at her clinic soon after her arrival, becoming an Associate Medical Director in 2017 and Medical Director in 2023. She describes her path to leadership as “by chance.” “I am a quiet leader; I observe the big picture and keep tabs on all the players. Being a leader for your organization is important; it sets a tone, and we need to have people who can make things happen,” said Slack.
Slack feels strongly that her health center offers her a fantastic career with options to grow. “FQHCs are places where you have lots of autonomy. Caring for underserved populations requires creativity and out-of-the-box thinking. You are still like an independent practitioner. You get to work with cool, passionate, mission-driven people, and you are allowed to find your niche. There will always be variety, and you can do it for a long time.”
CHC, Inc. will start the first Utah Teaching Health Center, a four-slot family residency located at CHC, Inc. and in rural sites in 2025