“50% of what you learn in medical school will be proven wrong.”

Figure 1. Is this person healthy? Despite what appearances may suggest, her labs show K 3.1 and WBC 4.1 from daily caloric restriction of approximately 900 cals, with no purging behaviors. These behaviors led to constant fatigue even before starting residency and losing 200 lbs of force on leg press after her body cannibalized muscle for fuel. Less than six weeks after this photo, she began anorexia treatment the same week as PR’ing a half-marathon. She started treatment almost seven years after she started meeting the criteria for (atypical) anorexia after having lost nearly 40% of her body weight.
This version of an apocryphal quote (attributed to many people, including William Osler and Carl Sandberg) was often repeated during my medical school education, including the start of our first lecture. The challenge, of course, is revealed in the rest of the quote — namely, that we don’t know which part it will be. Despite the quote’s repetition, we were rarely told the degree of confidence we could rely upon for each fact being shoved into our brains or how strong (or not) the evidence was behind the medicine.
Much like this quote, society and the medical system start to believe statements if they are repeated enough. It can then be challenging to unseat long-held beliefs, even after evidence is published to the contrary. What is common knowledge gets accepted as truth without questioning the underlying evidence basis or even the potential for implicit bias driving its origin.
Such as the much-vaunted BMI. The Body Mass Index (BMI) was created by a European actuary to determine the population statistics of Caucasian males. It was never intended for widespread dissemination nor clinical use.1 BMI was never validated on the overwhelming majority of the world’s population, i.e., females and non-Caucasians, and yet it is the defining characteristic of whether someone is “sick enough” to deserve treatment coverage for multiple diseases.
For example, the DSM-5 mandates that a patient must be underweight in order to receive the diagnosis of “anorexia,” and BMI is how the severity is defined — not the presence of other factors such as bradycardia, hypokalemia or low bone density, but purely on the BMI. This bias/distinction has also spawned the fatphobic diagnosis of “atypical” anorexia, in which a patient has all the characteristics of anorexia except for low BMI.2 This bias causes treatment initiation for “atypical” anorexia to be significantly delayed because of this distinction, despite the high mortality risk of eating disorders.3
In addition to the mental struggles a patient may face of not being “good enough” at having an eating disorder, insurance companies often deny coverage for things such as inpatient/residential stays or even regular dietician visits, purely due to coding F50.89 (other specified feeding and eating disorders) rather than F50.01 (anorexia nervosa, restricting type). A patient can be seen in a family physician’s office for fatigue after having lost 40% of their previous body weight through severe restriction, be congratulated for losing weight and then be told to lose more weight to treat their fatigue — true story.
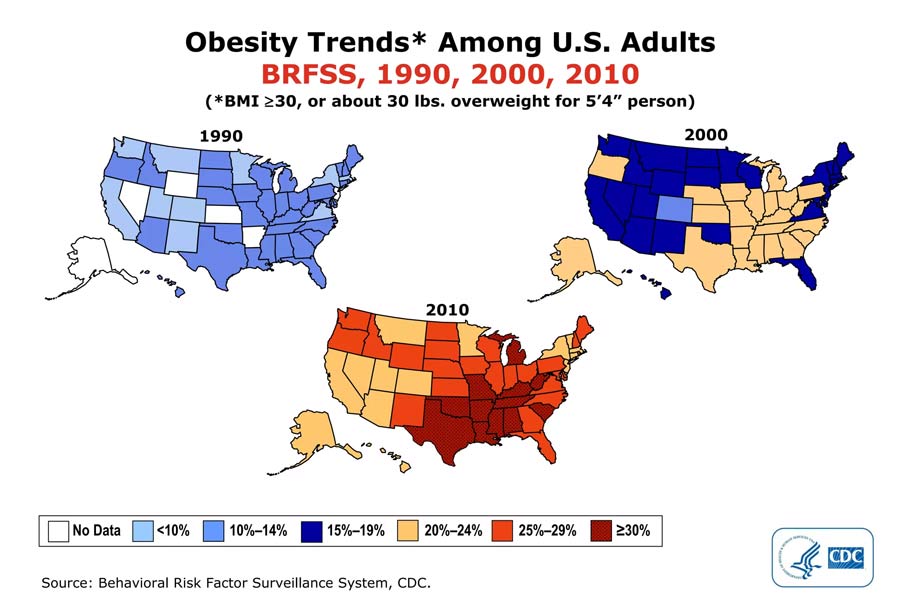
Or the creation of obesity as a disease. In addition to the BMI being extrapolated from its original purpose, being considered “normal,” “overweight” or “obese” is purely based on a patient’s BMI. For example, the population map showed a stark change in 1998, when the normal/overweight cutoff was lowered from 27.8 (men) or 27. 3 (women) to 25.4 The change was political, as studies actually showed that higher BMI was not associated with mortality until at least 40 was used as the cutoff.5,6 Ancel Keys, head of the Minnesota Starvation Experiment and also known food company spokesperson, was the one who advocated for BMI as the general measure of “fatness” without disclosing his conflicts of interest — after all, medicalizing someone at a higher weight opens up more opportunities to sell them weight-loss/health products! Actually, 77% of the NIH Obesity Task Force were weight-loss clinic directors,7 and the majority had multiple industry-related conflicts of interest.8
Yes, our country is getting heavier as the decades go by. Agreed — this is undeniable. There are many correlations with this increase, but we have all learned that correlation does not prove causation. We cannot prove a specific cause that lets every diet-plan sect blame their forbidden fruit of choice. We need to stop blaming individuals for our society’s changing body types. We ignore studies that show people at higher weight were more likely to have been infected with adenovirus-36 and that infecting multiple animal species with this virus led to increased weight gain and body fat without changes in their caloric intake.9,10
We also ignore the true magnitude of the “obesity epidemic.” The CDC published in JAMA that “more than 400,000 Americans died of overweight and obesity every year, so many that it may soon surpass smoking as the leading cause of preventable death.”11 The retraction, which was far less publicized, acknowledged that there were computational errors in the original study, so that “obesity and overweight were only associated with an excess of 26,000 annual deaths, far fewer than guns, alcohol, or car crashes.” In 2000, there were 86,000 fewer deaths than expected of people in the “overweight” category than if they were at a “normal BMI.” Furthermore, there were slightly more total deaths of people in the “Underweight BMI” category than those in both the “overweight” and “obese” categories.12
When we continue to blame the individual for a problem that is not completely a problem, we ignore the influences of social determinants of health, of racism, of misogyny. Just like healthcare institutions want to pretend that the individual physician who is burned out was not “resilient” enough rather than having to address systemic burdens, we also pretend that a person at a higher weight is “lazy” or doesn’t have enough willpower. Studies show that people at higher weights consume approximately the same amount or even fewer calories than lean people.13-16 The myth of “calories in, calories out” is just that — a myth.
Diets don’t work. It has been proven repeatedly that calorie restriction leads to higher weight rebound eventually,17-23 but the $5 billion health/wellness industry has a very vested interest in convincing us that “this one” will be the unicorn magic pill/diet/whatever that changes your life forever.
Or you can change your life forever by choosing to opt out of the diet mentality and get off that hamster wheel. Marketing machines don’t make any money with this approach because the opportunity to capitalize on the latest fad/gimmick/or program is eliminated.
Naomi Wolf says, “A culture fixated on female thinness is not an obsession about female beauty, but an obsession about female obedience. Dieting is the most potent political sedative in women’s history; a quietly mad population is a tractable one.”24
Enter Health at Every Size.25,26 Lindo Bacon, Ph.D., collated the studies in their groundbreaking book of the same name. They demonstrate that every body has a natural weight setpoint, even if it doesn’t align with our current guidelines as “healthy.”27 The body wants to return to that weight, regardless of what we eat/exercise.28 But if someone cannot control/lower their weight setpoint, then they should not be blamed as “lazy” or “noncompliant.” The next step is this radical concept: treat people without regard for their body size. Treat their medical conditions like diabetes and hypertension, certainly. But:
- Stop denying needed medical care (such as surgery or medication) until they lose weight.
- Stop encouraging weight loss since studies have shown repeatedly that diets don’t work.
- Recognize that we all deserve to take up space in this world — no one expects a Great Dane to look like or fit into a carrier intended for a chihuahua.
- Stop asking people to change their natural body characteristics because it makes others feel more comfortable.
- Start treating all people as human beings worthy of genuine care. Because we all are.
All bodies are good bodies, regardless of size, gender identity, race, level of disability, social status or any other method society has created to put people into boxes. Michigan is the only U.S. state that explicitly forbids fat discrimination.29 There is a very real benefit to being thin in this society: Fat people make less money than thin people.30 They are the subject of frequent micro- and macroaggressions. They are judged as “lazy” and “less than.” The prevalence of weight-based discrimination is now as common or more so than race- or gender-based discrimination.31-33 Is it any wonder that 30 million Americans are estimated to have an eating disorder in their lifetimes? Again, we need to stop blaming the individual for a systemic problem.
What can we do as family physicians?
Make clinic visits more accessible:
- Wider seats in all areas (so that all your patients and staff are comfortable)
- Seating available that has no armrests
- Sufficient weight limits on equipment
Reduce patient anxiety about clinic visits:
- Being weighed is a choice, except for when absolutely necessary (eg, weight-based dosing of a medication or e-prescribing for someone under 18)
- Don’t mention losing weight unless someone asks about it
- Don’t congratulate someone on weight loss — you don’t know what they went through to get there
- Treat them for their chief concern, not for their weight
- Remove “well-nourished” or mentions of BMI/weight-based terms from your physical exam template. People at a higher weight cringe when reading their notes because these terms are immediately perceived as an indictment of themselves.
The worse outcomes for people of heavier size almost disappear when correcting for microaggressions and social determinants of health.31,32,34-40 Health is not a function of your size.
Hypertension is a disease. Diabetes is a disease. Anorexia is a disease whose risk of mortality is based on the degree of disordered behaviors, not weight. Medical training and the healthcare community have taught us that being at a higher weight is a disease. Let’s recognize that last statement as being part of the 50% that gets later proven wrong. Let’s treat our patients as people deserving of care, no matter what their demographics.
Sara is a HAES-aligned family- and sports-medicine physician who practices at her clinic, The PEAAC, in Millcreek, UT. She specializes in treating people with eating disorders and performing artists/athletes/musicians. She serves as a Team U.S.A. doctor for U.S. Figure Skating, U.S.A. Gymnastics and U.S.A. Archery. You can reach Sara at sara@thepeaac.com or www.thepeaac.com.
References
- Nuttall FQ. “Body Mass Index: Obesity, BMI, and Health: A Critical Review.” Nutr Today. 2015. 50(3): 117-128.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). 2013.
- Harrop EN, Hutcheson R, Harner V, Mensinger JL, Lindhorst T. “’You Don’t Look Anorexic’: Atypical anorexia patient experiences of weight stigma in medical care.” 2023. 46: 48-61.
- National Institutes of Health. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report, 1998.
- Andres R. “Beautiful Hypotheses and Ugly Facts: The BMI-Mortality Association.” Obes Res. 1999. 7(4): 417-19.
- Troiano RP et al. “The Relationship between Body Weight and Mortality: A Quantitative Analysis of Combined Information.” Int J Obes Relat Metab Disord. 1996. 20: 63-75.
- Ernsberger P, Koletsky RJ. “Weight Cycling.” JAMA. 1995. 273(13): 998-99.
- National Institutes of Health National Task Force on the Prevention and Treatment of Obesity. “Long-Term Pharmacotherapy in the Management of Obesity.” JAMA. 1996. 276(23): 1907-15.
- Pasarica M et al. “Human Adenovirus Ad-36 Induces Adiposity, Increases Insulin Sensitivity, and Alters Hypothalamic Monoamines in Rats.” Obesity (Silver Spring). 2006. 14(11): 1905-13.
- Dhurandhar NV et al. “Human Adenovirus Ad-36 Promotes Weight Gain in Male Rhesus and Marmoset Monkeys.” J Nutr. 2002. 10: 3155-60.
- Mokdad AH et al. “Actual Causes of Death in the United States, 2000.” JAMA. 2004. 291: 1238-45.
- Flegal KM et al. “Excess Deaths Associated with Underweight, Overweight, and Obesity.” JAMA. 2005. 293(15): 1861-67.
- Wooley S, Wooley OW. “Should Obesity Be Treated At All?” Eating and Its Disorders, eds. Stunkard AJ, Stellar, EJ. New York: Raven, 1984.
- Garrow, JS. Energy Balance and Obesity in Man. New York: Elsevier, 1974.
- Braitman LE, Adlin EV, Stanton, Jr JL. “Obesity and Caloric Intake: The National Health and Nutrition Examination Survey of 1971-1975 (HANES 1).” J Chronic Dis. 1985. 38(9): 727-32.
- National Resource Council (National Academy of Sciences). “Diet and Health: Implications for Reducing Chronic Disease.” Ed. Committee of Diet and Health (Food and Nutrition Board/Commission on Life Sciences): National Academy Press, 1999.
- Coakley EH et al. “Predictors of Weight Change in Men: Results from the Health Professionals Follow-Up Study.” Int J Obes Relat Metab Disord. 1998. 22: 89-96.
- Bild DE et al. “Correlates and Predictors of Weight Loss in Young Adults: The CARDIA study.” Int J Obes Rel Metab Dis. 1996. 20(1): 47-55.
- French SA et al. “Predictors of weight change over two years among a population of working adults: The Healthy Worker Project.” Int J Obes Relat Metab Disord. 1994. 18: 145-54.
- Korkeila M et al. “Weight-loss attempts and risk of major weight gain.” Am J Clin Nutr. 1999. 70: 965-73.
- Stice E et al. “Naturalistic weight-reduction efforts prospectively predict growth in relative weight and onset of obesity among female adolescents.” J Consult Clin Psych. 1999. 67: 967-74.
- Shunk JA, Birch LL. “Girls at risk for overweight at age 5 are at risk for dietary restraint, disinhibited overeating, weight concerns, and greater weight gain from 5 to 9 years.” J Am Diet Assoc. 2004. 104(7): 1120‑26.
- Stice E, Presnell K, Shaw H. “Psychological and Behavioral Risk Factors for Obesity Onset in Adolescent Girls: A Prospective Study.” J Consult Clin Psych. 2005. 73(5): 195-202.
- Wolf N. The Beauty Myth: How Images of Beauty Are Used Against Women. HarperPerennial: 2002.
- Bacon L et al. “Evaluating a “Non-diet” Wellness Intervention for Improvement of Metabolic Fitness, Psychological Well-Being and Eating and Activity Behaviors.” Int J Obes. 2002. 26(6): 854-865.
- Bacon L. Health at Every Size: The Surprising Truth About Your Weight. Dallas: Benbella Books, Inc. 2008.
- Schwartz MW. “Brain Pathways Controlling Food Intake and Body Weight.” Exp Bio Med. 2001. 226(11): 978-81.
- Leibel RL, Rosenbaum M, Hirsch J. “Changes in Energy Expenditure Resulting from Altered Body Weight,” NEJM. 1995. 332: 621-28.
- “MI Weight Discrimination Claims.” Harvard T.H. Chan School of Public Health. https://www.hsph.harvard.edu/wp-content/uploads/sites/1267/2022/02/MI-Weight-Discrimination-Claims-4.pdf
- Picker L. “Why Obesity Lowers Wages.” Nat Bureau Econ Res. 2005. https://www.nber.org/digest/aug05/why-obesity-lowers-wages#:~:text=Prior%20studies%20generally%20have%20found,face%20significant%20labor%20market%20discrimination.
- Puhl R, Brownell K. “Bias, discrimination and obesity.” Obes Res. 2001. 9(12): 788-805.
- Puhl RM, Heuer CA. “The stigma of obesity: a review and update.” Obesity (Silver Spring). 2009. 17(5): 941-64.
- Puhl RM, Andreyeva T, Brownell KD. “Perceptions of weight discrimination: prevalence and comparison to race and gender discrimination in America.” Int J Obes. Mar 4 2008.
- Fontaine KR et al. “Body Weight and Health Care among Women in the General Population.” Arch Fam Med. 1998. 7(4): 381-84.
- Olson CL, Schumaker HD, Yawn BP. “Overweight Women Delay Medical Care.” Arch Fam Med. 1994. 3(10): 888-92.
- Amy N, Aalborg A, Lyons P, Keranen L. “Barriers to routine gynecological cancer screening for White and African-American obese women.” Int J Obes Relat Metab Disord. 2006. 30(1): 147-155.
- Flegal KM et al. “Overweight and Obesity in the United States: Prevalence and Trends, 1960-1994. Int J Obes. 1998. 22: 39-47.
- Brook RD. “Is Air Pollution a Cause of Cardiovascular Disease? Updated Review and Controversies.” Rev Environ Health. 2007. 22(2): 115-37.
- McEwen BS. “Protective and damaging effects of stress mediators.” NEJM. 1998. 338(3): 171-79.
- O’Neill EA, Trout K, Winter VR. “Relationships between experiencing anti-fat microaggressions, body appreciation, and perceived physical and mental health.” J Health Psych. 2022. 28(2).
- “Obesity Trends in the U.S.” Harvard T.H. Chan School of Public Health. https://www.hsph.harvard.edu/obesity-prevention-source/us-obesity-trends-map/








