Why Lung Cancer?
In the time it will take you to read this article, an estimated 34 people worldwide will die from lung cancer.1 In the United States alone, lung cancer results in 350 deaths per day. It’s expected to account for 21% of total cancer deaths in 2023, claiming the lives of 127,070 Americans.2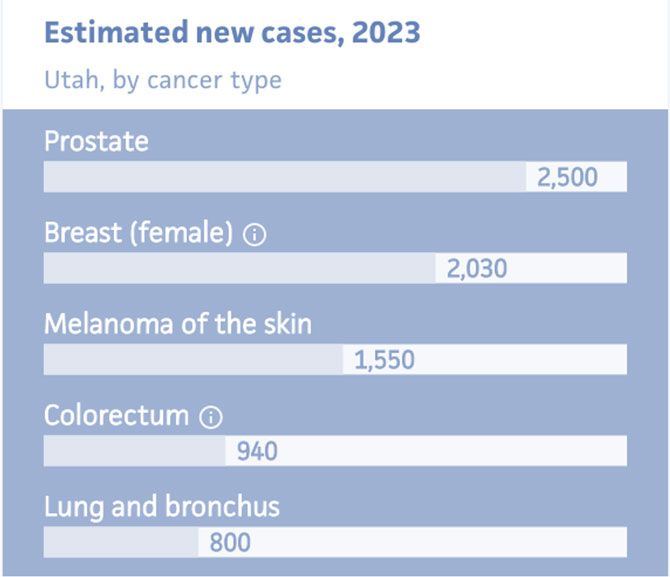
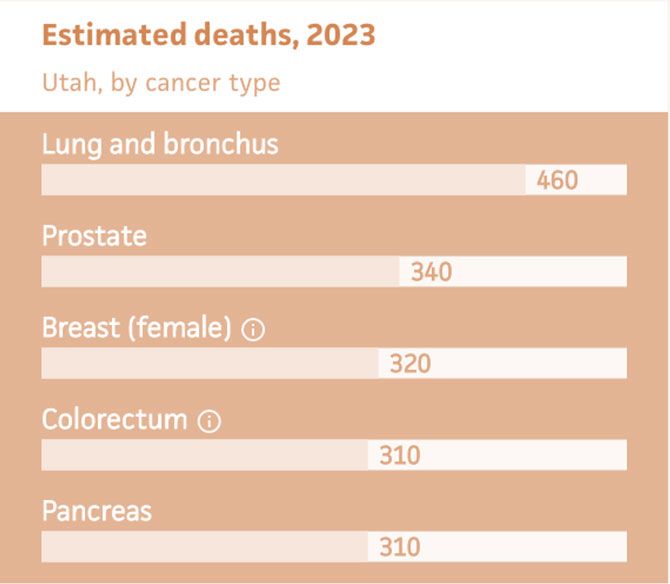
Figures 1 & 2: Adapted from American Cancer Society, Utah Cancer Statistics and Estimates 2023
Contrary to popular belief, lung cancer is the leading cause of cancer death in the United States and the world. It is estimated that about 6% of people will develop lung cancer during their lifetime in the United States. That includes about one in every 15 men and one in every 17 women.2
Lung cancer causes more deaths than breast, prostate, and colon cancer combined. Every year, there are about 50,000 more new cases of breast cancer than lung cancer, but lung cancer causes 90,000 more deaths than breast cancer. Despite significantly fewer cases, lung cancer kills three times as many women as breast cancer and three times as many men as prostate cancer.3
In Utah, lung cancer is the fifth most prevalent cancer but is the most deadly4 (see Figure 1).
What Makes Lung Cancer So Fatal?
The most common symptoms of lung cancer are chronic cough, coughing up blood, chest pain, and shortness of breath. Additional symptoms may include hoarseness, loss of appetite, fatigue, persistent lower respiratory infections, and a new onset of wheezing. However, these symptoms are usually indicative of the cancer’s progression into an advanced stage, where it is more difficult to treat and the prognosis is poor.5
If cancer can be detected before the patient becomes symptomatic, the five-year survival rate for patients with localized lung cancer is 61%. Unfortunately, only 19% of lung cancers are diagnosed at this early stage, whereas 55% are diagnosed once the cancer has metastasized, at which point the five-year survival rate drops to less than 9%.6 This is why early detection of lung cancer is so important; if we can detect lung cancer at an early stage, available treatment options and prognosis are both better.
The Current State of Lung Cancer Screening
The national screening rates for breast cancer, cervical cancer, and colon cancer average around 73%. However, in 2019, only 5.7% of high-risk individuals were screened for lung cancer, less than a tenth of the average for the other cancers.7
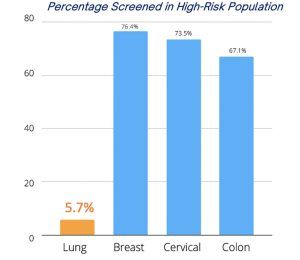
The low smoking rates in Utah may lead you to the conclusion that this is not our problem. On the contrary, only 2% of high-risk individuals in Utah were screened in 2022.8 This ranks us 45th as a state. Over the last five years, the lung cancer screening rate in Utah did not significantly change, but with your commitment, you can become an advocate for this cause and for your patients.
What Can Be Done?
The gold standard for lung cancer screening is a low-dose CT scan (LDCT). In an LDCT, only about 1–1.5 millisieverts of radiation are necessary,9 which is about a fourth of a full chest CT. A population-based randomized control trial initiated in 2000 entitled the NELSON trial, confirmed the life-saving benefit of lung cancer screening by LDCT.10 The NELSON trial consisted of two groups followed over the course of 10 years. A total of 13,195 men and 2,594 women between the ages of 50 and 74 were randomly assigned to periodically undergo LDCT screening or no screening.
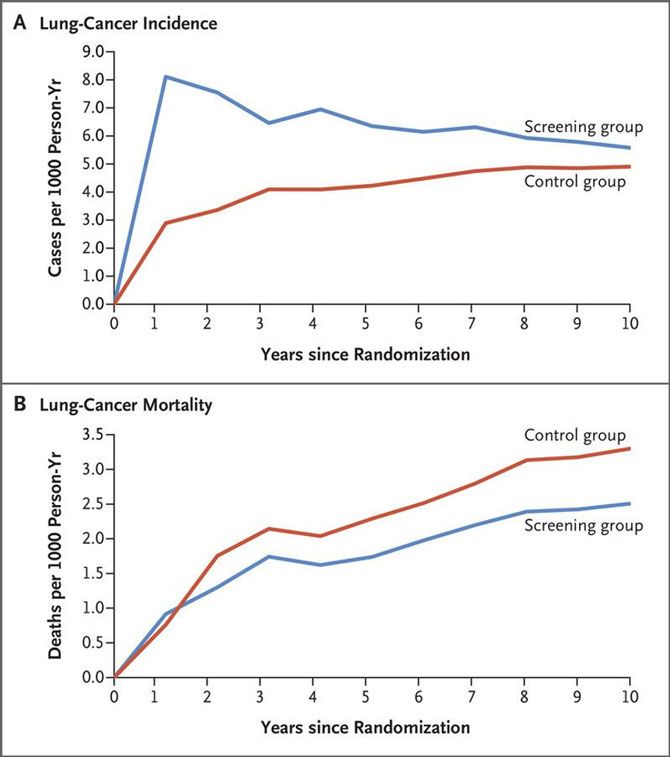
In the screening group, 58.6% of lung cancers were diagnosed at stage I; in the non-screening group, 13.5% of lung cancers were diagnosed at stage I. In the LDCT group, there was a 24% reduction in lung cancer mortality in men and a 33% reduction in lung cancer mortality in women when compared to no screening. Thus, early detection translates to a reduction in mortality.
Should Your Patient Be Screened?
In March 2021, the United States Preventive Services Task Force (USPSTF) updated the guidelines for lung cancer screening.11 According to current eligibility requirements, a person must:
- Be between age 50–80
- Currently smoke or have smoked in the past 15 years
- Have a 20 pack-year smoking history or greater
[Note: 1 pack-year = smoking 1 pack per day for a year]
While these new guidelines have nearly doubled the number of eligible individuals for lung cancer screening, they only include individuals with heavy smoking histories. There are other risk factors for lung cancer that are not accounted for in the current screening guidelines, such as secondhand smoke exposure and radon, that should be considered at the provider’s discretion.12
If your patients are eligible, it is recommended that they get screened for lung cancer annually.
About Us: What is ALCSI?
The American Lung Cancer Screening Initiative (ALCSI) is a 501(c)(3) non-profit raising awareness about lung cancer and lung cancer screening. Part of the reasoning behind the low screening rates in the U.S. is that 84% of those eligible for lung cancer screening are not familiar with the low-dose CT.13 Our goal is to change that.
We believe that educating communities about lung cancer and screening is crucial to reducing lung cancer mortality. We aim to educate a variety of audiences about lung cancer screening. By working together with primary care physicians like you, we hope to change the trajectory of lung cancer screening for good.
To learn more, please visit our website: https://www.alcsi.org
Anne Clark is the Education Chair for the Utah Chapter of ALCSI and has lived in Utah for the past 14 years. She is a senior at BYU studying Neuroscience and is applying to medical school this year.
References
- Piñeros M, Mery L, Soerjomataram I, et al. Scaling Up the Surveillance of Childhood Cancer: A Global Roadmap. JNCI: Journal of the National Cancer Institute. 2020;113(1):9-15.
- Siegel RL, Miller KD, Wagle NS, et al. Cancer statistics, 2023. CA Cancer J Clin. 2023;73(1):17-48.
- Society AC. Cancer Facts and Figures 2023 Available: https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/2023-cancer-facts-figures.html.
- Society AC. Utah Cancer Statistics Available: https://cancerstatisticscenter.cancer.org/#!/state/Utah.
- Detterbeck FC, Nicholson AG, Franklin WA, et al. The IASLC Lung Cancer Staging Project: Summary of Proposals for Revisions of the Classification of Lung Cancers with Multiple Pulmonary Sites of Involvement in the Forthcoming Eighth Edition of the TNM Classification. J Thorac Oncol. 2016;11(5):639-650.
- Institute NC. Cancer Stat Facts: Lung and Bronchus Cancer Available: https://seer.cancer.gov/statfacts/html/lungb.html.
- National Cancer Institute N, HHS, Bethesda, MD. Cancer Trends Progress Report. October 2022.
- Association AL. State of Lung Cancer: Utah Available: https://www.lung.org/research/state-of-lung-cancer/states/utah.
- Rampinelli C, De Marco P, Origgi D, et al. Exposure to low dose computed tomography for lung cancer screening and risk of cancer: secondary analysis of trial data and risk-benefit analysis. Bmj. 2017;356:j347.
- Ru Zhao Y, Xie X, de Koning HJ, et al. NELSON lung cancer screening study. Cancer Imaging. 2011;11 Spec No A(1a):S79-84.
- Force USPST. Final Recommendation Statement: Lung Cancer Screening Available: https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening.
- Schabath MB, Cote ML. Cancer Progress and Priorities: Lung Cancer. Cancer Epidemiol Biomarkers Prev. 2019;28(10):1563-1579.
- Soneji S, Yang J, Tanner NT, et al. Underuse of Chest Radiography Versus Computed Tomography for Lung Cancer Screening. Am J Public Health. 2017;107(8):1248-1250.








