I grew up in Provo, attended Timpview High School, was an All-State cross country and track athlete, and trained under Hall of Fame coach Brian Kuhlmann. I turned down scholarship offers at multiple schools and competed at BYU as a preferred walk-on, fulfilling a lifelong dream of wearing the cougar uniform. After a church mission in Brazil, I decided that my racing days were over, and it was time to focus on school. I regularly tell my adolescent patients that my high school GPA was 2.94 and my college GPA was 3.85, hoping to help them gain self-confidence and to recognize their own potential, even though they have failed classes.
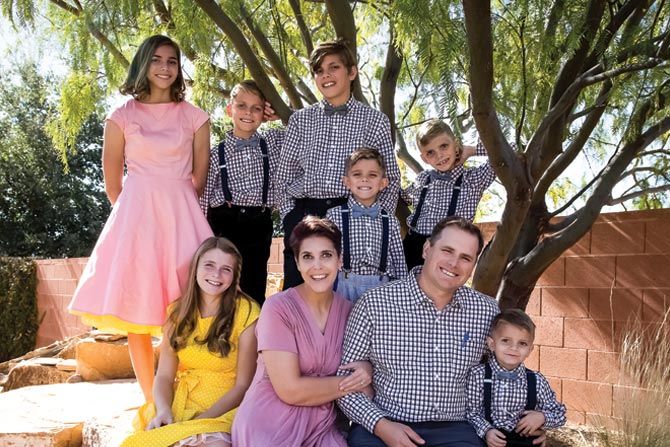
My wife Annalisa and I met at the BYU bookstore, where I was price-checking economics textbooks for my textbook arbitrage business. I thought she was cute, so I introduced myself and asked for her phone number, and the rest is history. We are the proud parents of seven children. She continues to be the single most important story in my history.
I am the high school baseball pitching coach at Karl G. Maeser Preparatory Academy, which is my second part-time job (albeit unpaid). Having never played the sport, I’ve spent way too much time reading textbooks, articles, and medical literature to help me craft my coaching. We finished second in UHSAA 2A this year, and my pitchers had the lowest ERA in the league. I have a special focus on injury prevention for throwing athletes and organized free online training for coaches and athletes.
My other part-time job (still, unpaid) is to live broadcast sporting events. This is my favorite hobby, and I consider myself a modern-day one-man band. I do commentary, run the scoreboard overlays, switch the music, and change the camera angles for the six cameras I strategically place around the playing area, all from my lawn chair.
The Journey to Become a Physician
As I mentioned, I attended BYU as an undergrad and majored in economics. I attended medical school at A.T. Still University in Mesa, Arizona and served as Chief Resident at Southern Illinois University Family Medicine Residency in Carbondale. I come from a family of nurses and physicians, so I had cousins and grandparents I revered as a child. I never really remember a day when I said, “I’m gonna be a doctor.”
My greatest mentor in college was my organic chemistry professor, Steven Fleming, who never directly answered my questions, but always guided me to find my own answers. My most influential preceptor in medical school was my OB/GYN preceptor, Douglas Gates, MD, as he showed me superior skills in doctoring by establishing a lasting doctor/patient relationship. My most inspirational leader was my residency program director, Penny Tippy, MD, who gave me the freedom to pursue my educational interests as a resident.
Choosing Family Medicine
As a fourth-year medical student, I was doing a site visit in Kentucky for a triple board Psych/Peds/CAP residency program, and it seemed perfect for me. The next Monday morning, I started my ER rotation, and while I didn’t enjoy the short-lived relationships in the ER, I was reminded how much I loved diagnostic medicine and changed
my plan.
My FM preceptors, hearing my interest in psychiatry and pediatrics, counseled me that I could manage a large practice of FM patients with mental health needs, as well as care for pediatric patients. Their guidance was paramount in this decision process.
The most attractive aspect of family medicine is the long-lasting doctor-patient relationship and family relationships. While serving the population of Parowan, UT, for three years, I loved caring for entire extended families, mom/dad/cousins. I spend much of my new patient visits taking a social history, as I sincerely want to know about the patient and who they are outside
the clinic.
Going the Extra Mile for Patients
One unique element of my practice is my house call practice. During my residency, the daughter and primary caregiver of one of my chair-bound patients suddenly died. Uncertain about how to get my patient into the clinic, I asked where he lived, trying to work out transportation, and I was made aware that he lived just across the street. From then on, all our visits took place in his living room, and the benefit to him was incredible. I decided to try to do home visits for my homebound patients, if possible.
Leading up to the COVID-19 vaccine release, I had many encounters with patients where I spoke of hope for a vaccine, but also, in reality, I didn’t expect one until the next year or later. When the vaccine was approved earlier than expected, I remained positive and encouraging in my communications with my patients.
But I was frustrated for many of my senior patients, as they lacked the resources to schedule an appointment online. Most didn’t have a computer, and those who did just weren’t fast enough to get those precious appointments that disappeared faster than a BTS concert ticket. So I decided to schedule the visits for them.
As a value-based physician, I had a list of my patients and their annual healthcare expenses. I sorted by cost and started from the top down, using expenses as a surrogate marker for poor health. When I got a “10-minute reservation” to schedule an appointment, I would have my nurse enter the patient’s information as I quickly dialed their phone number. If they didn’t answer on the first call, we moved on to the next patient. It was a very fast-paced race to get as many scheduled as possible. If the patient answered, I’d say, “this is Erik. I have a vaccine appointment for you next week at 3 PM. Can I book you now for it?” They sensed my urgency, and their response was almost always significant joy that I had thought of them. I told them my nurse would call later with the details, and I hung up and moved on to the next patient.
The health department released new vaccine appointments every week at a specific date and time, and if you were lucky, you could schedule one appointment per week. I learned a handful of tricks to improve the odds of getting an appointment slot, and within two weeks of practice, I was an expert at scheduling appointments. It required me to spend an extra one to two hours a night, but I was regularly scheduling 30 vaccine appointments every time the health department released appointments. I made and shared a video online for all to see my tricks so others could also get appointments for their loved ones.
After all was done, my staff and I scheduled hundreds of appointments for our patients. And while my practice has been shown, through modeling, to be one of the most complex family medicine practices in the area, I’ve only had two patients end up in the ICU throughout the entire pandemic due to COVID-19. My theory is that this is because of early vaccine acceptance in my practice and good hand hygiene.
The Future of Family Medicine
As family physicians, we need to be open to precepting medical students. FM doctors, at least in my circles, were never trained to teach medical students in the clinic and improve efficiency. For years I said that medical students added two hours to my day. Now, I see them as valuable members of my team that help care for the patients in their own different ways. I think students should take aptitude tests, and we should encourage these. It will help point medical students to a specialty that will make them happiest. That may not be primary care, but that is
all right.