Introduction
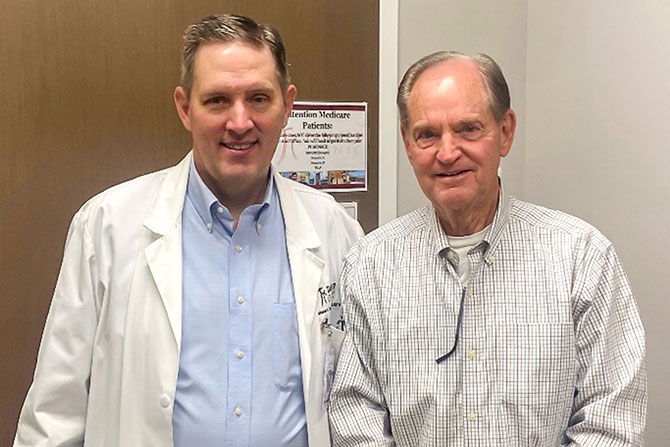
D.G. is a 79-year-old Caucasian male. He is a retired educator who taught political science and law at the high school level. The patient presented with a three-week history of slurred speech and some difficulty completing his weekday golf game. He was concerned that after a few minutes of talking, he sounded like Elmer Fudd and his “wascally wabbit” pattern of speech. D.G. was also worried about his ability to give a talk at his local church within the coming weeks due to the worsening dysarthria. He also complained about some difficulty closing his lips fully and reported dribbling when brushing his teeth. Upon physical examination by his family physician, he noted some weakness of the eye while mouth closure was strong. There was no external ophthalmoplegia — eye movements were normal and there was no ptosis. However, there was some fatigability of the proximal limb muscles, deltoids, and hip flexors. Due to the symptoms, he was concerned that this could possibly be Myasthenia Gravis (MG), especially with the dysarthria that came with prolonged speech. D.G. was referred to a neurologist who ordered labs, including an Acetylcholine receptor panel for diagnosis.
Discussion
Neuromuscular junction disorders can be genetic, such as congenital myasthenic syndromes, or caused by external toxins like botulinum toxin and curare. Others are acquired autoimmune conditions, including MG, Lambert-Eaton myasthenic syndrome (LEMS), and neuromyotonia.1 MG is the most common neuromuscular disorder and presents primarily with muscle weakness and fatigue.4 It is an autoimmune, B-cell-mediated disease in which antibodies attack key proteins, such as acetylcholine receptors (AChR), muscle-specific kinase (MuSK), LRP4, agrin, titin, and ryanodine.1 Due to its clear mechanism and location of action, Myasthenia Gravis is not only a prototype for autoimmune diseases but also a valuable model for understanding synaptic function.
MG is categorized into subtypes based on clinical features and antibody profiles, including early-onset MG, late-onset MG, thymoma-associated MG, MuSK, LRP4, seronegative, and ocular MG.1 Although it is a rare disease, the number of Myasthenia Gravis cases has been rising over the past two decades, particularly among the elderly. This increase is likely due to improved availability of antibody testing and a growing aging population.5 It affects individuals of all ages, sexes, and ethnic backgrounds, though it is most commonly seen in young adult women under the age of 40 and older men over the age of 60.3 Despite its prevalence across various populations, Myasthenia Gravis is neither inherited nor contagious, although in rare cases, more than one member of a family may be affected.
The underlying pathophysiology of MG involves antibodies that exert their influence on skeletal muscle acetylcholine receptors and impede the normal function of acetylcholine at the neuromuscular junction.3 This disruption impedes normal muscular contraction, leading to fluctuating muscle weakness and fatigue. The thymus gland, which plays a central role in immune system development during childhood by producing T-lymphocytes, is often implicated in the pathogenesis of Myasthenia Gravis. While the thymus normally atrophies after puberty, in many adults with MG it remains enlarged and may contain clusters of lymphoid tissue.1 Some individuals may also develop thymomas. The thymus is thought to contribute to the autoimmune process by generating autoreactive T cells that direct the production of pathogenic antibodies against the acetylcholine receptor.
Common features of Myasthenia Gravis include3:
- Eye muscle weakness causing ptosis and diplopia.
- Bulbar weakness causing dysarthria and dysphagia.
- Dyspnea.
- Limb weakness.
- Fatigability.
All of these features can wax and wane, often worsening as the day goes on or with sustained activity.
There are a few ways to diagnose myasthenia gravis which include3:
- Blood tests.
- The main blood test used is very sensitive and specific: acetylcholine receptor antibodies of which there are three types — binding, blocking and modulating. Some labs will only run two of the three.
- While uncommon, MUSK is another blood test used. This is almost nonexistent in Utah, but can help diagnose young Black women.
- Electrophysiology, specifically repetitive nerve stimulation, can be performed.
- Single-fiber EMG.
- Imaging, a CT to look for a thymoma, however not useful for diagnosis of MG.
- A trial of Mestinon can also help in confirming diagnosis.
As seen, there are a few ways to help recognize MG; however, antibody testing has revolutionized its diagnosis.
Treatment2
While there is no cure, the following treatments can manage symptoms effectively:
- Medications:
- Pyridostigmine (brand name Mestinon) is used as a first line, with immediate effect.
- Steroids.
- Immunosuppressive drugs like azathioprine (brand-name Imuran).
- Vyvgart, a new medication that may work with a variety of autoimmune diseases; however, it is very expensive.
- IVIG: These are short-term treatments used in some cases.
- Very rare, but a thymectomy in which surgical removal of the thymus gland may improve symptoms or lead to remission in some cases.
Myasthenia Gravis is treated differently by different specialists but is relatively gratifying to treat, often responding to meds.
Conclusion
Upon meeting with the neurologist, the initial concerns of MG in the patient were confirmed through the AchR Panel. D.G. was prescribed pyridostigmine, which he is responding well to. He reported that he is able to golf five days a week, give talks in church and no longer sounds like he is hunting wabbits.
- Bubuioc, A.-M., Kudebayeva, A., Turuspekova, S., Lisnic, V., & Leone, M. A. (2021). The epidemiology of myasthenia gravis. Journal of Medicine and Life, 14(1), 7–16. https://doi.org/10.25122/jml-2020-0145
- Farmakidis, C., Pasnoor, M., Dimachkie, M. M., & Barohn, R. J. (2018). Treatment of myasthenia gravis. Neurologic Clinics, 36(2), 311–337. https://doi.org/10.1016/j.ncl.2018.01.011
- Myasthenia gravis. (n.d.). National Institute of Neurological Disorders and Stroke. Retrieved April 6, 2025, from https://www.ninds.nih.gov/health-information/disorders/myasthenia-gravis
- Phillips, L. H., 2nd. (2003). The epidemiology of myasthenia gravis. Annals of the New York Academy of Sciences, 998(1), 407–412. https://doi.org/10.1196/annals.1254.053
- Thanvi, B. R., & Lo, T. C. N. (2004). Update on myasthenia gravis. Postgraduate Medical Journal, 80(950), 690–700. https://doi.org/10.1136/pgmj.2004.018903