Feature Image: Dr. Frank Powers and patient
Imagine you had the opportunity to create your ideal family medicine residency from scratch. Given that family physicians mostly work in community settings, you’d likely situate your ideal residency in a community-based primary care setting, where most learning occurs through caring for continuity patients. Ideally, the residency might be sponsored by a community health center, rather than a hospital system, so as to maximize focus and institutional resources on a single program. You’d also want to ensure that your residents care for a highly diverse patient population, representing multiple languages and cultures. Furthermore, your residents — especially those wanting to work in rural areas — would need experience working in high-volume tertiary care centers to gain emergency medicine, obstetrics, and inpatient medicine experience. Perhaps most importantly, you’d want the funding for the residency to go directly to your program, instead of sharing funds among a multitude of competing departments.
Though this vision may seem too good to be true, creating and supporting such primary care residencies is the explicit goal of the Teaching Health Center Graduate Medical Education (THCGME) program. Since 2010, the THCGME program has funded over 81 community-based residencies which have trained over 2,000 primary care physicians and dentists. To date, Utah has not benefited from this program; though this is about to change. In July 2025, the new Community Health Centers Family Medicine Residency (CHCFMR) will welcome their first class of incoming residents. The program will be the first THCGME program in the state, aiming to train primary care physicians specifically to work in rural and underserved areas.
Utah Continues to Suffer Primary Care Workforce Shortages
Family physicians can particularly impact health outcomes in rural and underserved areas. Access to a regular primary care physician has been linked to lower infant mortality, higher birth weights, immunization rates exceeding national standards, reduced healthcare costs, and longer, healthier lives.
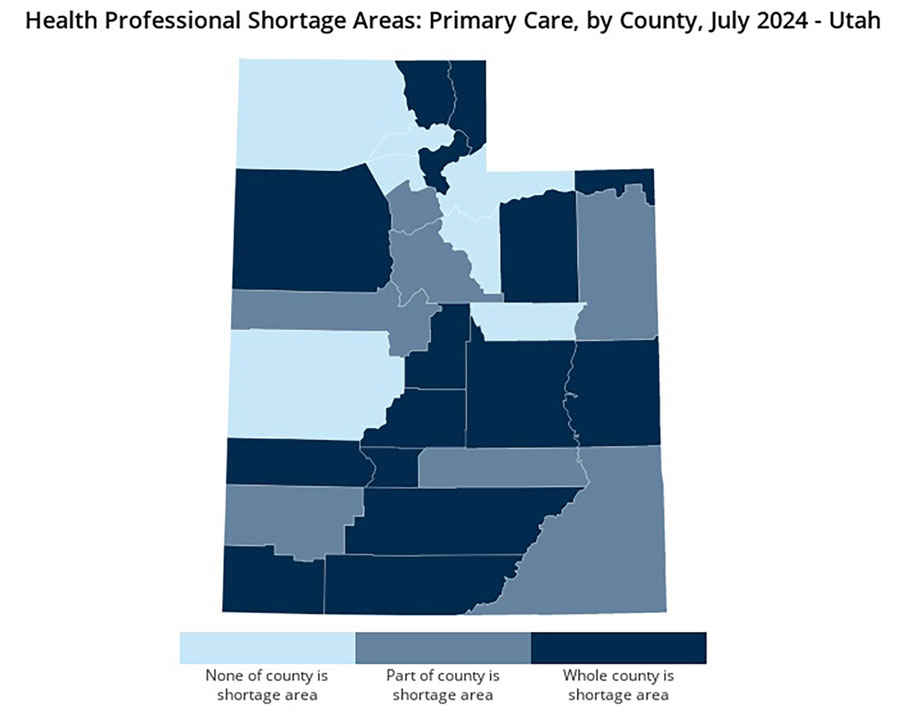
Yet, the Bureau of Health Workforce projects a shortage of 68,020 full-time equivalent primary care physicians by 2036 in the United States. Shortages are particularly profound in Utah’s rural and underserved populations: Across the state, Utah has fewer primary care providers per population (5.8 per 10,000) than the U.S. average (7.6 per 10,000). Utah has the lowest percentage of active primary care physicians in the United States, with a projected need for 123.9 primary care physicians per year. Additionally, 30.3% of Utah family physicians are over 60 years old, contributing to workforce gaps in the coming decades. Utah’s projected population growth (4 million people by 2030) and the increase in aging patients will increase needs for physician supply.
Rural Utah, which comprises 83% of the state’s counties, has significantly fewer primary care providers compared to urban areas; 21.5% of the state’s population lives in rural areas, yet only 11% of the state’s primary care providers practice in such areas. Health disparities exist across racial and ethnic lines in Utah as well, and have worsened in the last 20 years, particularly among Hispanic/Latino, Black/African American, and Native Hawaiian/Pacific Islander populations. These disparities lead to poorer health outcomes across multiple realms of health.
Despite these needs, and a significant increase in medical students graduating from Utah schools (currently 475 annually), there remain a small number of family medicine residency positions (29 annually) available in the state. The state’s existing residencies provide outstanding clinical training and retain the majority of graduates within Utah, yet are nonetheless inadequate in size to meet current and physician workforce needs.
The THCGME Program Helps Communities Grow Their Healthcare Workforce
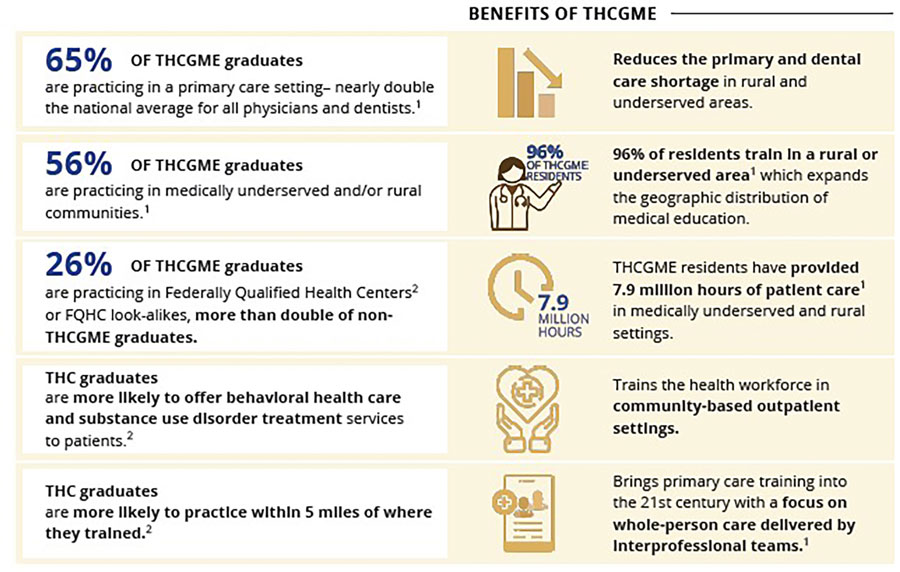
The THCGME program is a unique national program which aims to change the resident training paradigm by providing the majority of training in community-based outpatient settings.
THCGME programs are primary care residencies housed at Federally Qualified Health Centers (FQHCs), rural health clinics, or tribal sites. The program dates from 2010, when a portion of the Affordable Care Act allocated $230 million over five years directly to community-based ambulatory primary care centers, instead of hospitals as was typical for Graduate Medical Education Funding previously. Since that time, the THCGME program has grown substantially and has made a meaningful impact on physicians working in rural and underserved settings.
As of 2021, the THCGME program boasts a total of 59 new primary care residencies (since 2010 PH) and has trained over 1,200 family physicians. Of all THCGME graduates, 56% practice in medically underserved or rural communities, often practicing in a broader scope, including substance use treatment (MAT with buprenorphine), behavioral health care, outpatient gynecology, and obstetrics. Residents spent the majority (96%) of their training in medically underserved communities. Among 2022 graduates, 34% reported coming from disadvantaged or rural backgrounds and 20% from underrepresented in minorities in medicine
Furthermore, the THCGME program is highly cost-efficient. By focusing on training physicians to provide high-quality, cost-conscious care, the program has saved $1.8 billion in federal healthcare expenditures between 2019 and 2023.
Community Health Centers Inc. Sponsors Utah’s First THCGME
Community Health Centers Inc. (CHC) is Utah’s largest federally qualified health center. CHC operates six clinics in Salt Lake County and two in Box Elder County, caring for a diverse urban underserved population. In addition to providing primary care to 35,000-40,000 patients — most of whom are served in a language other than English, and over 50% of whom do not have insurance — CHC has a robust maternal-neonatal service line, delivering over 1,400 babies annually at LDS and the University of Utah Hospitals. Because of their diverse patient population and broad spectrum of practice, CHC physicians have been actively involved in teaching medical students, residents, and APC students from other institutions, for decades.
In 2022, a group of family physicians at CHC led by Drs. Frank Powers and Andy Garrison devised a plan to start a new family medicine residency to address the workforce shortage in Utah, expand access to care, and address the specific needs of medically underserved communities. Having worked at CHC for over a decade, including during the COVID-19 pandemic, they had witnessed firsthand workforce turnover, increased individual workloads, and limits on access to care. And they were all directly involved in medical education — as a group CHC physicians have been involved with medical education as teaching faculty for students and residents at the University of Utah for over 40 years. This seemed like a natural next step and the funds from the federal Teaching Health Center Planning and Development Program and Utah state primary care development grant made this possible.
Starting in May 2023, CHC embarked on the process of program development and ACGME accreditation with enthusiastic support from partners at Intermountain LDS Hospital, Primary Children’s Hospital, the University of Utah Health, Utah AHEC (Area Health Education Centers), and AUCH (Association of Utah Community Health), including from current and former family medicine residency program directors in Utah. Our intent is to complement rather than compete with existing Utah family medicine residencies and work in collaboration to expand family medicine training opportunities in Utah — each program offers something unique to potential residents. The CHC Family Medicine Residency (CHCFMR) received accreditation on October 24 and will accept the first class of residents in July 2025.
Importantly, as a federally qualified health center, CHC is governed by a board composed of at least half of the health center patients. During the residency planning and development process, the CHC board and leadership worked closely alongside residency faculty, ensuring that the residency will ultimately remain accountable not just to the ACGME, but to the very patients served by future residents.
The CHCFMR Will Focus on Training Residents for Rural and Underserved Practice
The CHC Family Medicine Residency Program will train 12 residents (four per year) in diverse, underserved outpatient primary care settings across both urban and rural areas. In addition to their outpatient experience at CHC — where most patients are served in a language other than English, and over 90% are at or below 200% of the federal poverty level — residents will complete specialty and inpatient rotations at LDS Hospital and Primary Children’s Hospital, and affiliated clinical sites throughout the Salt Lake Valley. The program will have a particular focus on preparing residents for rural and/or underserved practice, including developing skills in behavioral health care, substance use disorder treatment, obstetrics and neonatal care, and outpatient gynecologic procedures. CHC’s broad scope of practice, coupled with the CHCFMR’s robust curriculum, will ensure that, upon graduation, residents are highly prepared for rural and/or underserved practice.
By incorporating training in both rural and underserved settings in Utah, the CHCFMR will provide both the clinical skills residents need to provide high‑quality care to such populations, as well as relationships with physicians throughout the state to support graduate retention.
Graduates working in these underserved areas will be eligible for student loan repayment programs including HRSA NHSC (National Health Service Corps), further supporting primary care physician retention in rural and medically underserved areas. By 2050, CHCFMR will have graduated 88 family physicians practicing in medically underserved areas in Utah.
Yet, the impact of the CHCFMR is not limited to its graduates. Given that residents will provide patient care to an urban underserved population in the family medicine practice during residency, they will have a direct impact on access to care. In one year, among all programs nationally, 932 THCGME residents treated 792,000 patients during more than 1.2 million patient encounters. We project that, when the CHCFMR has the full complement of 12 residents, this will increase CHC’s capacity by 8,400 outpatient encounters annually. Furthermore, like other THCGME programs, CHCFMR will provide more access to telehealth, opioid use treatment, and integrated services in the service area. And by the nature of our practice model at CHC, CHCFMR will increase access to pregnancy-related care and pediatric care. CHCFMR enables us to increase access to healthcare in our patient population.
Future Opportunities
We need the support of all family physicians and family medicine advocates. THCGME Funding is awaiting appropriation in Congress — you can contact your House and Senate representatives now to support this program. While the vast majority of CHCFMR resident rotations and experiences are in place, the program will only be strengthened by further community partnerships. Whether you are a physician in a rural or urban area, if you are interested in collaborating to train the Utah workforce of the future, please contact us. Individual family physicians can also contribute to addressing primary care needs as mentors and clinical preceptors for medical students, undergrad and high school students, as role modeling has a strong influence on career choice. Finally, CHC Family Medicine Residency demonstrates there is opportunity for others to develop new or expand current primary care training programs. There is potential to grow and expand CHC Family Medicine Residency at the current site or in new sites, or to start new Teaching Health Center residencies. HRSA continues to award Rural Residency Planning and Development grants. And many states have successfully used state funds, including Medicaid, to support primary care residency programs and, in turn, grow the physician workforce and expand access to care to their citizens — an opportunity Utah could explore.
We are members of a specialty integral to the health and wellness of our communities. The next generation is ready to join us, and we can provide them training opportunities to accomplish these goals.
For more information, visit our website at residency.chc-ut.org or email us at residency@chc-ut.org.









